MCheck NetworkIQ
AI to optimize the “three Cs” of network management: Compliance, Competitiveness, and Cost of Care
Curate the most competitive and cost-effective network with accurate provider recruitment sourcing and steer members towards high-performing providers whether to rapidly enter new markets or ensure proactive network adequacy compliance.
Optimizing provider networks every day across health plans
>57%
Reduction of ghost networks with no impact to adequacy
>56%
Reduction in time to close provider gaps
>0%
Cost savings over legacy vendors
Building a Competitive Network with AI
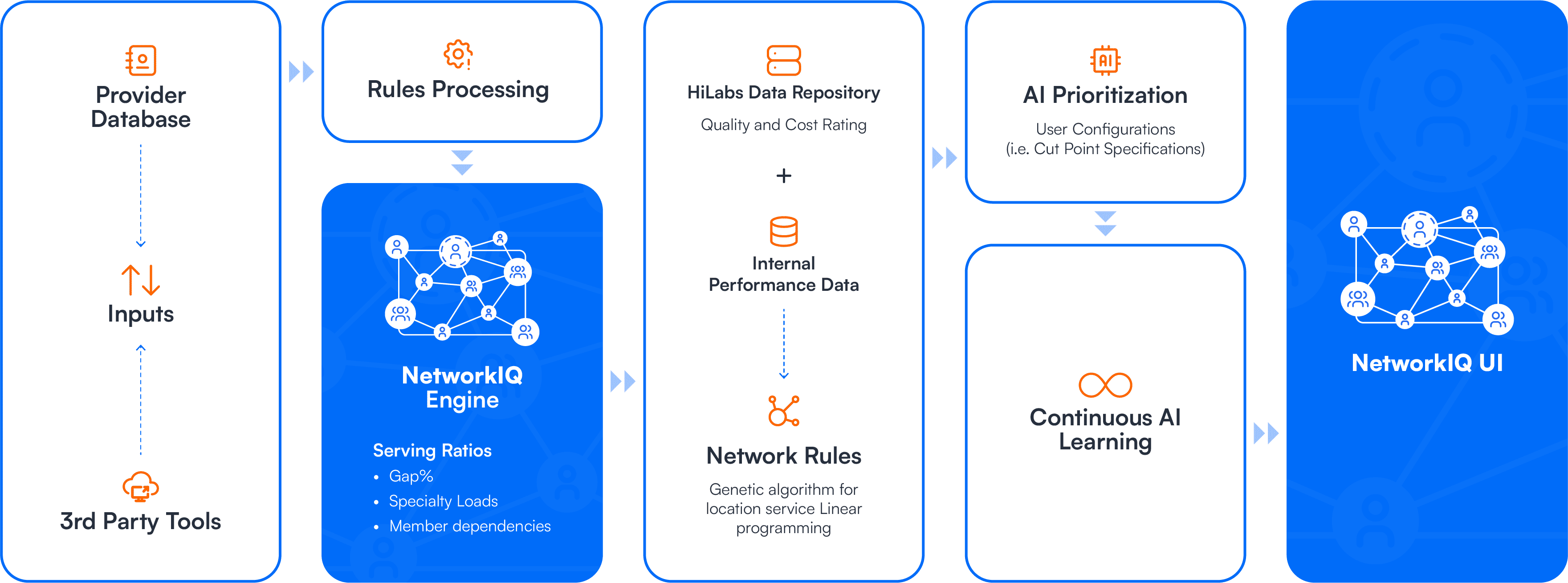
Why invest in AI-powered Network Management Solutions
Platform Capabilities
Data Sources & Integration
Insights & Analytics
Flexibility & reporting
User Interface
Platform Capabilities
Data Sources & Integration
Insights & Analytics
Flexibility & reporting
User Interface
Traditional
Disparate tools for compliance, modeling, and market intel lead to data silos and high administrative overhead
HiLabs
Unified platform with single sign-on for end-to-end provider network management and strategy
Grounded in Accuracy: How our solution stands apart
HiLabs AI-powered network management solution enables payers to stay compliant, rapidly enter new markets, and reduce cost of care

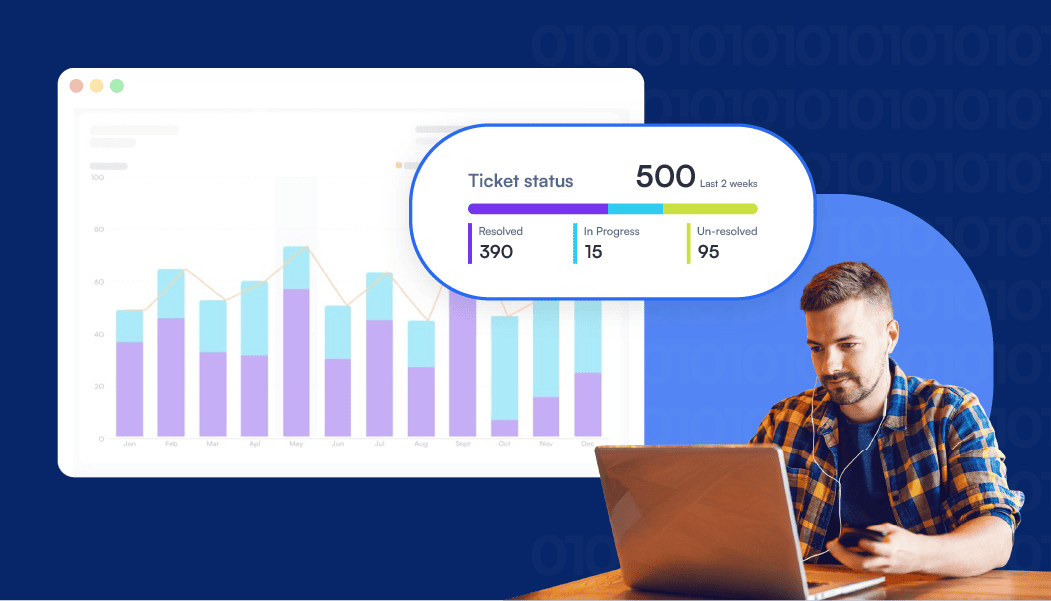
Ensuring Compliance with AI-Powered Network Adequacy
Audit Ready Templates & Reporting
Seamless, audit-ready regulatory reporting with pre-built CMS HSD outputs and state-compliant file submissions
Compliance Check
Pre-configured rules engine delivers real-time updates on CMS and market-specific regulations, reducing compliance risks and ensuring accuracy
Ensuring Compliance with AI-Powered Network Adequacy
Ghost-Network Elimination
Real-time “what-if” scenario modelling and provider cleansing with no impact to network adequacy
AI for Adequacy
AI-powered network adequacy analysis with smart gap closure to ensure CMS and state compliance
Smarter, Faster Network Expansion
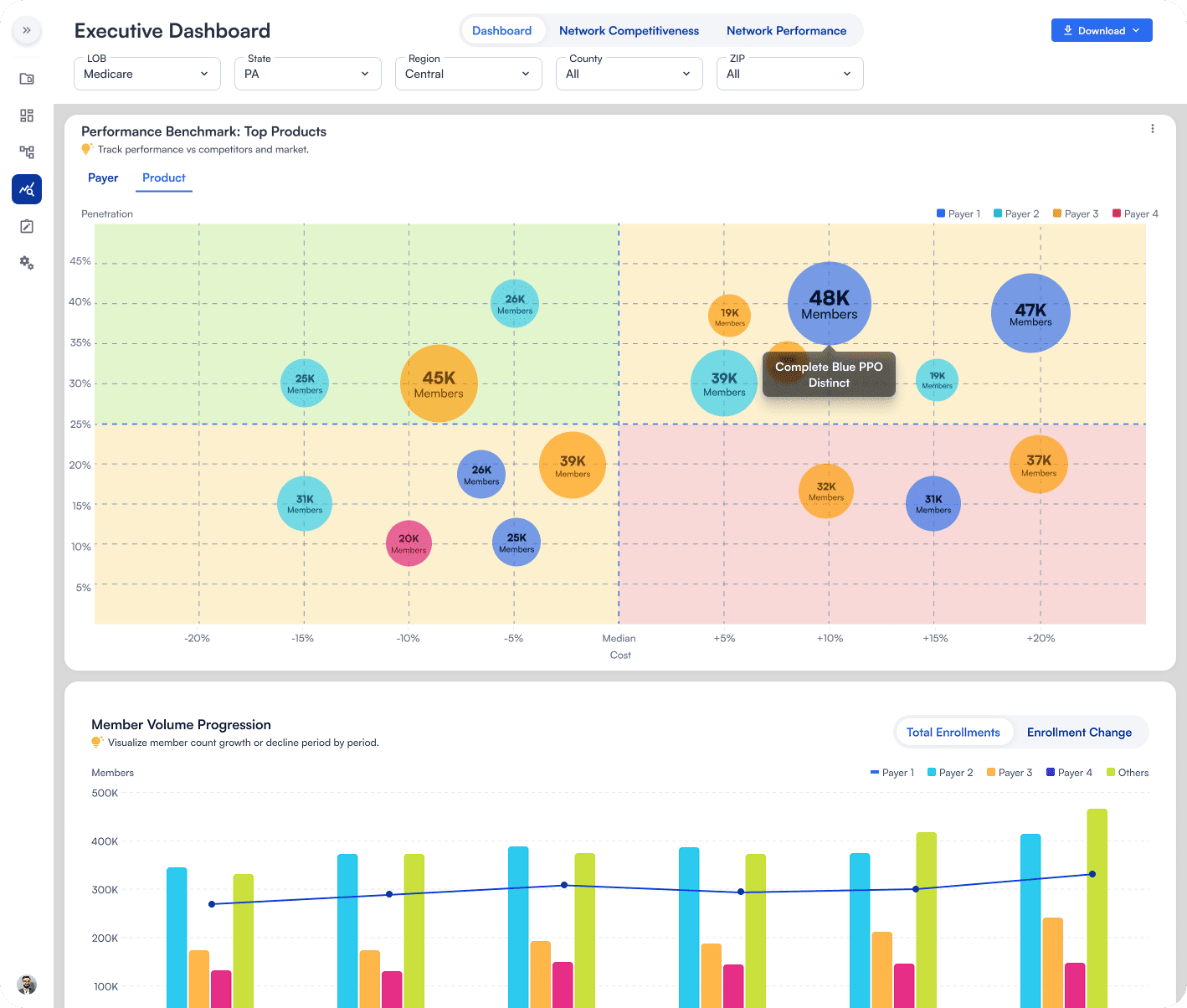
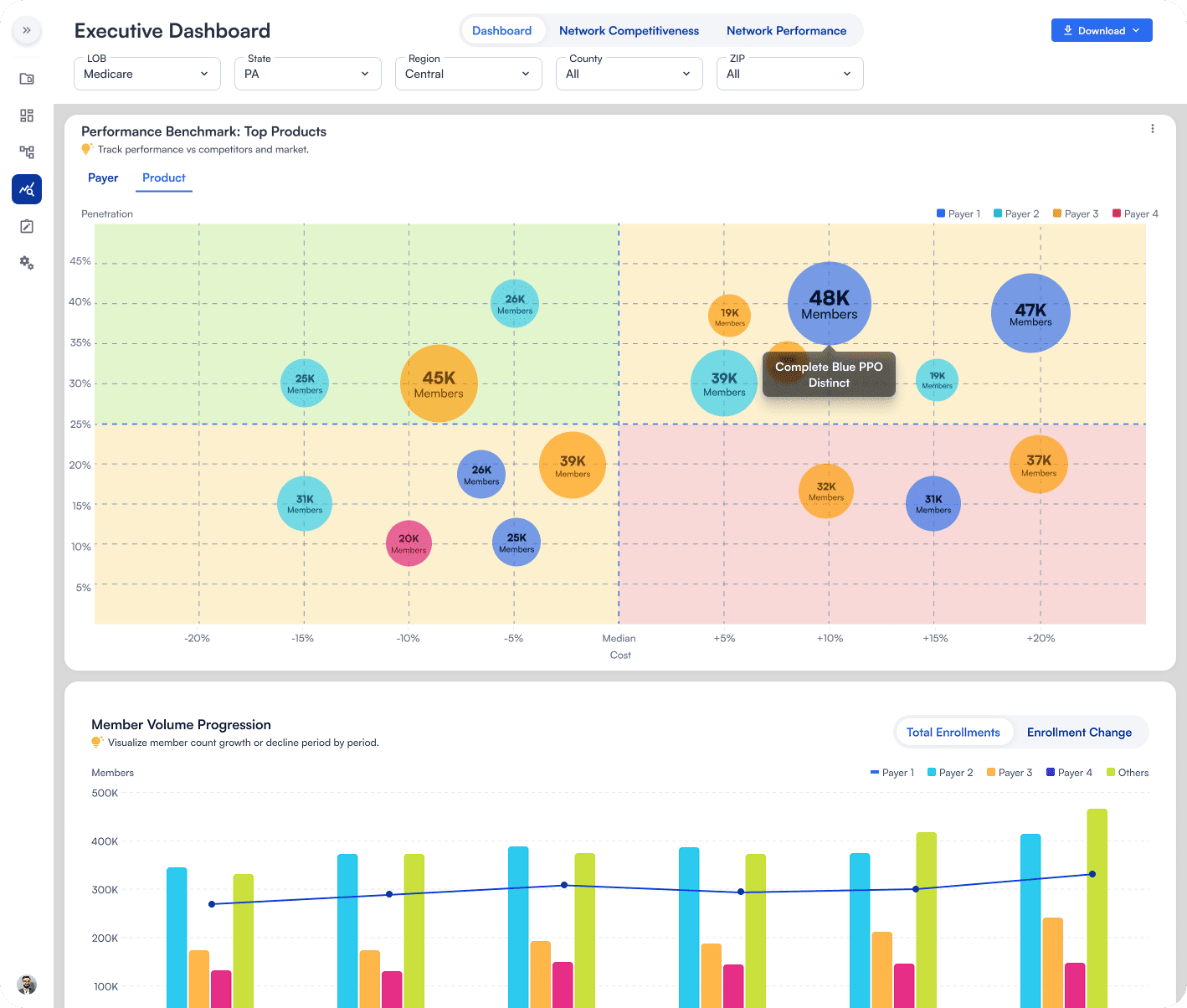
Competitive Intelligence
Precision-driven payer vs. payer comparisons for strategic network design across provider penetration and product benefit design
Network Disruption Forecasting
Proactively identifies drivers and financial implications of provider turnover, contract termination, and reimbursement negotiations against competitors
Smarter, Faster Network Expansion
Reimbursement Reconciliation
Uncover negotiation opportunities by benchmarking against geographic specific competitors and providers
Auto-Curating High-Performing Networks
Cost of Care Compass
360° View of a provider’s cost of care index in conjunction with its utilization to determine quality practice and appropriate practice scores
Network Steerage
Proprietary provider scoring algorithm that identifies high and low performing providers and facilities by leveraging clinical, member, claims, and pricing data for holistic provider performance evaluation
Auto-Curating High-Performing Networks
Referral Management
Analyzes referral patterns and patient leakage and keepage to improve member experience and outcomes as well as reduce out-of-network spend
Discover how a national plan leveraged AI-powered insights to enhance network adequacy
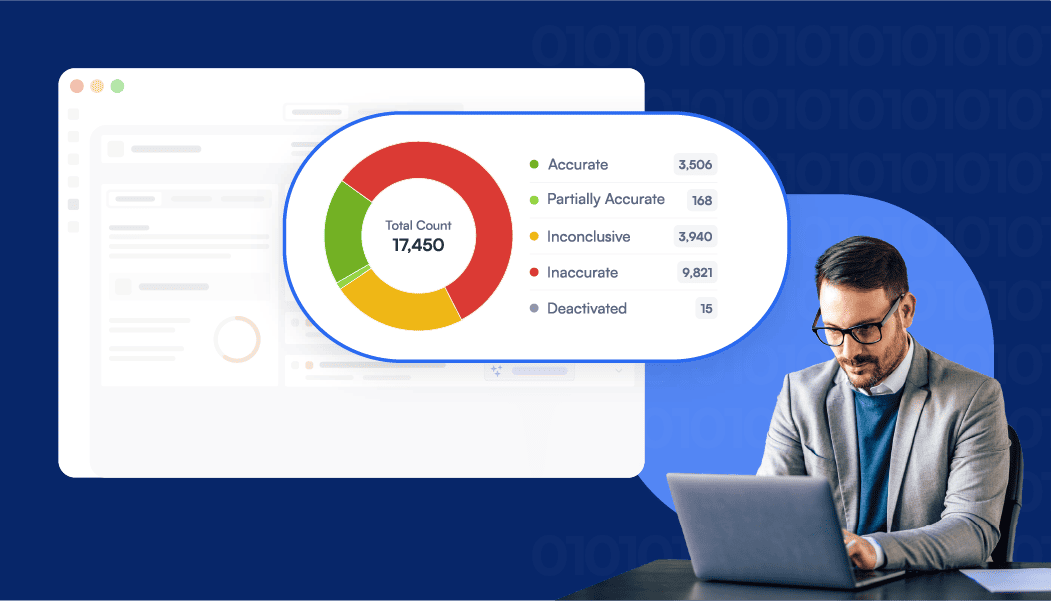
Ghost Network Modelling: 97%+ Cleansing Rate with Zero Compliance Risk
HiLabs AI-powered R3 algorithm, featured in JAMA, leverages 1000s of publicly available sources in real time combined with advanced geospatial technology to cleanse over 97% of ghost networks with no impact to payor network adequacy
High-Value Provider Sourcing for Gap Closure: 95%+ Accuracy
HiLabs AI-powered NetworkIQ auto-recommends high-performing and marketable providers for optimal network design while ensure network adequacy compliance
Cost Efficiency: 40% Savings Over Legacy Vendors
HiLabs automates data validation, multi-source aggregation, and adequacy analysis in one platform—cutting costs by 40% and replacing fragmented, manual legacy processes
MCheck Platform
Explore Other MCheck Solutions